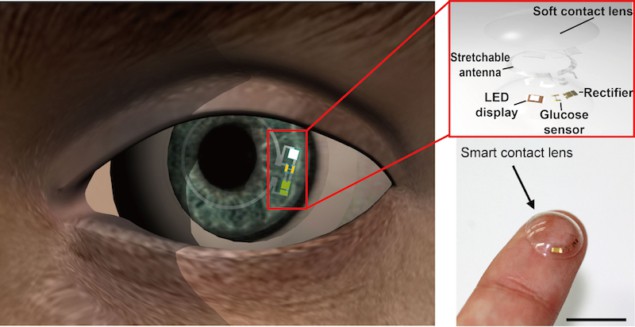
A new, soft, flexible contact lens can monitor glucose levels in tears wirelessly and even alert the user if glucose levels are too high by turning off a light-emitting diode embedded in the device. The lens, which has already been successfully tested out on live rabbits, could be used to screen for pre-diabetes and in non-invasive real-time health monitoring applications for diabetics.
Researchers have developed a variety of wearable and non-invasive sensors in recent years. These include electronic-skin coatings that can detect blood oxygen levels, contact lenses made from metal-oxide thin films that can detect glucose levels in tears and flexible integrated sensor arrays based on plastic and silicon integrated circuits that can detect molecules like glucose in sweat.
Most of the contact lens made so far, however, contain brittle and hard components fabricated on plastic films that can block the user’s vision and sometimes even damage the eye. They also often require bulky electronics to measure signals from the sensors, which of course is not very practical.
A team of researchers led by Jang-Ung Park of the Ulsan National Institute of Science and Technology (UNIST) in the Republic of Korea has now succeeded in making soft contact lenses in which glucose sensors, wireless power transfer circuits and LED display are integrated using transparent and stretchable nanostructures. The elastic parts of lens are formed using a silicone elastomer, a material widely used in soft contact lenses today.
Highly transparent and low haze
“Obviously, contact lenses should not obstruct the wearer’s view either, and they must be both highly transparent and have a low haze for optical clarity,” explains Park. “For the hybrid substrate of our lens, we thus used heterogeneous materials whose refractive indices do not vary very much and which match that of local areas of the eye. This ‘index-matching’ approach provides the wearer with a clear view – that is, outstanding transparency (93% in the visible light regime) and low haze (1.6% in the visible light regime).
“What is more, we maximized the elastic portion (a conventional soft contact lens material, as mentioned) so that it covered nearly 97% of the total area of the contact lens. This material allows oxygen to pass through it, thus making it more comfortable for the wearer.” The new set up avoids the need for additional, external measuring equipment and the wireless circuitry responds to glucose concentrations in moisture naturally found in the eye thanks to a sensor made of graphene. The sensor displays this information through the LED and if it is above a certain threshold (0.9 mM), it turns off, so providing a useful warning system to the wearer.
Towards industrialization and commercialization?
The researchers chose 0.9 mM of glucose as a threshold for diagnosing diabetes but this value can be changed by simply changing the resistance of the sensor. As the concentration of glucose in tear fluid increases, the resistance of the sensor decreases and this reduction in turn decreases the resistance of the parallel circuit of the LED and the sensor. This results in the reduction of the bias applied to the circuit so that it reaches a value that is below its turn-off voltage, so turning the LED off.
The researchers say that they have already successfully tested out their device on live rabbit eyes. The animals showed no “abnormal behaviour” during the tests, they say, and the lens remained in place.
“Thanks to the fact that the lens is made using rapid moulding and conventional photolithography techniques, it could easily be produced on the large scale,” Park tells nanotechweb.org. “We believe that it might be commercialized in the next five years, if companies are interested in investing in the device,”
The new lens is detailed in Science Advances DOI: 10.1126/sciadv.aap9841.